Technological Advances in Next-Generation Bone Grafts
What is a bone graft?
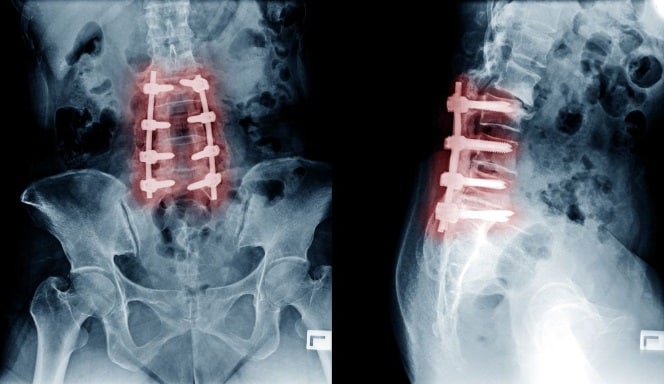
Bone graft is commonly used in spine and orthopedic surgical procedures. Bone grafting can be defined as a process where a supplemental material is placed into spaces around a fracture repair or around a fusion site or bone deficiency to aid in healing. Uses may include repair of unhealed fractures (non-unions), as a supplement to healing in loss of bone mass due to high energy fractures or tumors, or in promotion of fusion of bone segments in a spine or other joint fusion. The ideal bone graft material provides the following three functions: 1) osteoconductive property – a supportive scaffold to support new bone formation, 2) osteoinductive property – a molecular signal to promote new bone formation, and 3) osteogenic property – presence of bone forming cells to facilitate new bone formation.

What are the sources of bone grafts?
The first available bone graft source was autologous bone graft sourced from a patient’s own iliac crest pelvic bone or other alternative donor areas. This autologous graft provided all three desired functions of a bone graft but had limitations of potential surgical harvest complications and pain at the donor site. Alternatives to autologous bone grafts were developed such as synthetic bone graft material manufactured in the lab and bone allograft from a deceased human donor source. The goal of any alternative form of bone graft is to maintain as many of the three properties from autologous bone grafts as possible.
What are synthetic bone grafts?
Synthetic bone graft material reproduces the osteoconductive properties in a laboratory. This synthetic material is composed of varying amounts and types of calcium to form a filler compound which would act as a scaffold for new bone formation in the bone repair process. Advances have been made to the synthetic material to improve its osteoconductive properties. Recent advances included the addition of carbonate apatite (anorganic bone mineral), bioactive glass and Type I collagen fibers.
What are bone allograft products and DBMs?
Bone allograft products are harvested from a deceased donor in an approved regulatory manner. The allograft is processed, sterilized, and morselized to enable placement around the bone repair site. To further advance allograft options, demineralized bone matrices (DBMs) were developed. These allografts are processed to remove the cellular matrix and to partially remove the mineral matrix but in a method that retains the collagen matrix. This process preserves the native growth factors in the bone, such as bone morphogenetic proteins (BMPs) and other cell stimulation factors. Thus, DBMs provide both osteoinductive potential and an osteoconductive scaffold. These grafts do not maintain a cellular osteogenic component for bone healing.
What are “next generation” osteoinductive DBM allografts?
The next generation of these osteoinductive DBM allografts involve cleanroom processing with a low bioburden. This process eliminates the need to use hydrogen peroxide or high dose gamma sterilization which can reduce the effectiveness of the bone morphogenic proteins. The processing of these next generation DBMs delivers a product that is 100% bone without a glycerin carrier that is present in other commercially available products
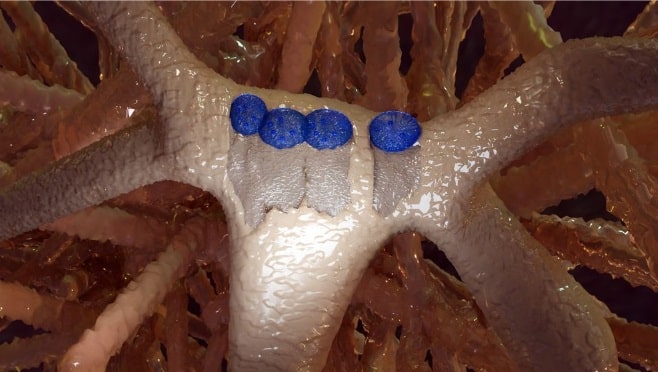
What are cellular bone grafts?
The third group of bone grafts have osteogenic properties in addition to osteoconductive and osteoinductive properties. They are often referred to as cellular bone grafts. In order to preserve cell viability upon harvest from a deceased donor, the allograft must be prepared and frozen within twelve hours. A cryoprotectant material is required for the allogenic cells to survive the freeze and thaw process. The purpose of cryopreservation is to maintain cell viability at extremely low temperatures for long-term storage and transport, such that the cells may be thawed at the time of surgery and provide benefits at the bone grafting site.
What are the risks of using DMSO?
Most of the available cellular bone grafts use dimethyl sulfoxide (DMSO) as an intracellular cryoprotectant. There is a concern of potential post thaw toxicity for DMSO which effects the cellular component of viable graft material and can be cytotoxic to the host tissue adjacent to the graft. These products must rely on washing or decanting of the extra DMSO prior to implanting. Residual amounts of DMSO may remain even after washing or decanting as DMSO is an intracellular cryoprotectant. Products that do not use DMSO as a cryoproctant are considered safer and more attractive to physicians and hospitals.
How are cells preserved in a cellular bone graft?
The next generation of these cellular bone allografts uses a proprietary cryo-preservative that protects the cells by bio-coating the cell membrane during the freeze and thaw process. This preservative is not cytotoxic and does not require rinsing or decanting for implantation.
When it comes to bone grafts, there is a wide array of options with varying compositions, properties, and sources. The selection of a bone graft material is dependent on the clinical situation and the surgeon’s preference among the available products.
To learn more about commercially available synthetic, allograft, and cellular bone graft products, please visit https://sanaramedtech.com/surgical/
References:
Tally WC, Temple HT, Burkus JK. Lateral lumbar interbody fusion using a cellular allogeneic bone matrix in the treatment of symptomatic degenerative lumbar disc disease and lumbar spinal instability. J Spine Surg. 2021 Sep;7(3):310-317. doi: 10.21037/jss-21-28. PMID: 34734135; PMCID: PMC8511570.
Gianulis E, Wetzell B, Scheunemann D, Gazzolo P, Sohoni P, Moore MA, Chen J. Characterization of an advanced viable bone allograft with preserved native bone-forming cells. Cell Tissue Bank. 2023 Jun;24(2):417-434. doi: 10.1007/s10561-022-10044-2. Epub 2022 Nov 25. PMID: 36434165; PMCID: PMC10209280.
Martin WB, Sicard R, Namin SM, Ganey T. Methods of Cryoprotectant Preservation: Allogeneic Cellular Bone Grafts and Potential Effects. Biomed Res Int. 2019 Oct 16;2019:5025398. doi: 10.1155/2019/5025398. PMID: 31737666; PMCID: PMC6817928.
Darveau SC, Leary OP, Persad-Paisley EM, Shaaya EA, Oyelese AA, Fridley JS, Sampath P, Camara-Quintana JQ, Gokaslan ZL, Niu T. Existing clinical evidence on the use of cellular bone matrix grafts in spinal fusion: updated systematic review of the literature. Neurosurg Focus. 2021 Jun;50(6):E12. doi: 10.3171/2021.3.FOCUS2173. PMID: 34062506.




