Prevention of microbial biofilms on implantable materials in vitro with BIASURGE™ Advanced Surgical Solution
Authors: Larry Estlack, Rebecca McMahon, PhD, Nina Bionda, PhD


I. Introduction
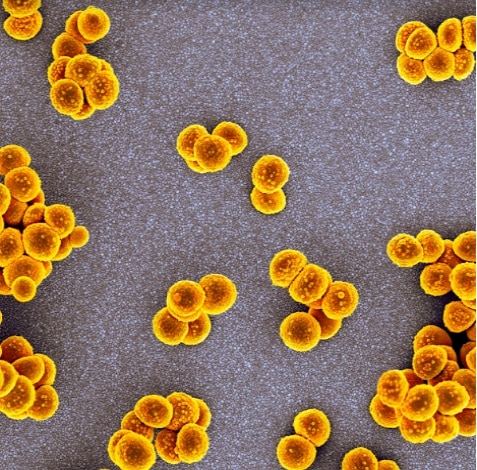
Biofilms are complex communities of bacteria which reside within an exopolysaccharide matrix adhered to biotic or abiotic surfaces.1 In the clinic, biofilms are associated with nosocomial, chronic, and device related infections.2,3 Due to the intrinsic antibiotic tolerance and development of antibiotic resistance, biofilms are notoriously difficult to treat.4 With the rapid advancements in the development of implantable devices and the risks of device contamination, the issue of implant-associated infections is garnering significant interest.3,5 These infections affect patients’ quality of life, contribute significantly to patient morbidity and mortality, and pose a high burden to the healthcare system.
This white paper presents the results of a series of in vitro studies aimed at evaluating both prevention of microbial colonization of four different implantable materials, as well as eradication of bacteria already attached to the surface of these materials. The experimental methodology, considerations, and findings are discussed in detail below.
The results demonstrate that BIASURGE Advanced Surgical Solution significantly reduces the bioburden on a variety of materials in vitro, both in the prevention and in the eradication model.
II. Methodology
Four different implantable materials in shape of coupons ½’’ in diameter were used in this testing: stainless steel (SS), cobalt-chromium alloy (CoCr), titanium alloy (Ti-6AL-4V), and ultra-high molecular weight (UHMW) polyethylene. The coupons were acquired from a commercial source (BioSurface Technologies Corporation, Bozeman, MT) and used without additional surface modifications. Coupons were glued to the bottom of 12-well plates using medical grade silicone adhesive. Two pathogenic bacteria were used as model organisms, Gram-positive methicillin-resistant Staphylococcus aureus (MRSA) ATCC BAA-1717 and Gram-negative Pseudomonas aeruginosa ATCC 9027. Schematic of the experimental set up is shown in

Figure 1. Schematic representation of the experimental set up.
©2023 Sanara MedTech. All rights reserved. MKT.15.09 231118
Prevention model: To evaluate effectiveness of BIASURGE Advanced Surgical Solution in preventing attachment of bacteria (Figure 1A), the coupons were first exposed to BIASURGE for 10 minutes followed by a wash twice with PBS and addition of 3×106 CFU of bacteria in full strength growth broth. Following 10 minutes of contact time with the inoculum, the coupons were detached from the plate and the bacteria present on the material was recovered through a series of sonication debridement steps. The bacteria were enumerated using standard serial dilution and agar plating methodology.
Eradication model: To evaluate effectiveness of BIASURGE Advanced Surgical Solution in disrupting preformed biofilms (Figure 1B), the coupons were first inoculated with approximately 106 CFUs of bacteria and incubated at 37°C for 24 h to allow formation of immature biofilms. The non-adhered bacteria were removed through washing with PBS and the coupons were then subjected to a 10 minute treatment with BIASURGE. Enumeration of bacteria remaining on the material surface was performed as described above.
III. Results
The results of the prevention assay are summarized in Figure 2A and demonstrate that BIASURGE Advanced Surgical Solution is effective at preventing microbial attachment to a variety of implantable surfaces. Pre-treatment of all four materials evaluated in this study with BIASURGE Advanced Surgical Solution resulted in at least 5-log reduction of the bioburden introduced onto the materials.

Figure 2A. Prevention model- results
©2023 Sanara MedTech. All rights reserved. MKT.15.09 231118


Figure 2B. Eradication model- results
In the eradication model where disruption of preformed biofilms was evaluated (Figure 2B), treatment of 24 h old biofilms with BIASURGE Advanced Surgical Solution again resulted in approximately 5-log reduction of the bioburden from all four materials evaluated.
IV. Conclusions
BIASURGE Advanced Surgical Solution is a no-rinse irrigation solution based on the synergistic mechanism of action of a combination of EDTAs, PHMB, and vicinal diols.6 Considering that microbial attachment is the critical first step in surface colonization and subsequent biofilm formation, we designed a series of studies to evaluate the use of BIASURGE Advanced Surgical Solution in the presence of a variety of implantable materials and simulated microbial contamination scenarios. The findings of the in vitro studies discussed here demonstrate that BIASURGE Advanced Surgical Solution is:
• Effective at significantly preventing attachment of bacteria to a variety of implantable materials. • Effective at significantly reducing existing bioburden from the surface of a variety of implantable materials.
The data shown here, coupled with the rapid microbicidal efficacy of planktonic microorganisms shown in the kill-rate study7, demonstrate the potential for BIASURGE Advanced Surgical Solution to make a clinical impact in reducing complications due to implant-associated infections. Targeted clinical studies are being designed to confirm this hypothesis.
©2023 Sanara MedTech. All rights reserved. MKT.15.09 231118

V. References
1. Costerton JW, Lewandowski Z, Caldwell DE, Korber DR, Lappin-Scott HM. Microbial biofilms. Annu Rev Microbiol. 1995; 49: 711-45.
2. Khatoon Z, McTiernan CD, Suuronen EJ, Mah TF, Alarcon EI. Bacterial biofilm formation on implantable devices and approaches to its treatment and prevention. Heliyon. 2018; 4(12): e01067.
3. Arciola CR, Campoccia D, Montanaro L. Implant infections: adhesion, biofilm formation and immune evasion. Nat Rev Microbiol. 2018; 16(7): 397-409.
4. Sharma, D., Misba, L. & Khan, A.U. Antibiotics versus biofilm: an emerging battleground in microbial communities. Antimicrob Resist Infect Control 8, 76 (2019).
5. Stoodley P., Hall-Stoodley L., Costerton B., DeMeo P., Shirtliff M., Gawalt E., Kathju S. 2013. Biofilms, Biomaterials, and Device-Related Infections, Handbook of Polymer Applications in Medicine and Medical Devices; 77–101.
6. Salamone AB, Salamone JC, McMahon RE, Poleon S, Bionda N, D’Arpa P. Synergistic Effect and Antibiofilm Activity of a Skin and Wound Cleanser. Wounds. 2020; 32(8): 208-216.
7. Estlack L, McMahon, RE, Bionda, N. Evaluation of Microbicidal Efficacy of BIASURGE™ Advanced Surgical Solution. 2020; white paper, data on file




