Treating a Post-Surgical Seroma or Hematoma
 A hematoma is generally defined as a collection of blood outside of blood vessels. It occurs because the wall of a blood vessel (artery, vein, or capillary) has been damaged, and blood has leaked into tissues where it does not belong. Hematoma is the term used to describe bleeding which has more or less clotted, different from hemorrhage which signifies active, ongoing bleeding. A bruise, for example, is actually a hematoma. During surgery, hematomas are caused by an injury to the wall of a blood vessel, prompting blood to seep into the surrounding tissues. Your surgeon will seal blood vessels as they are cut and will double-check those seals before closing the incision.
A hematoma is generally defined as a collection of blood outside of blood vessels. It occurs because the wall of a blood vessel (artery, vein, or capillary) has been damaged, and blood has leaked into tissues where it does not belong. Hematoma is the term used to describe bleeding which has more or less clotted, different from hemorrhage which signifies active, ongoing bleeding. A bruise, for example, is actually a hematoma. During surgery, hematomas are caused by an injury to the wall of a blood vessel, prompting blood to seep into the surrounding tissues. Your surgeon will seal blood vessels as they are cut and will double-check those seals before closing the incision.
Who is at risk of developing a seroma or hematoma?
The risk of a hematoma is much higher in patients who have been taking blood thinners and in those with some preexisting diseases or bleeding disorders. Vigorous coughing or marked elevation in blood pressure immediately after surgery may also contribute to the formation of a surgical site hematoma. Other risk factors include trauma, vigorous exercise, straining, vomiting, stress, and alcohol consumption. This is part of the reason it is so important to follow your doctor’s instructions.
What are some characteristics of a hematoma?
A hematoma produces elevation and discoloration of the surgical wound edges, discomfort, and swelling. Blood sometimes leaks between skin sutures. There may be pain and a feeling of fullness in the affected area. Depending on the site, there may even be visible bruising. Hematoma formation following operations on the thyroid, parathyroid, or carotid artery can be particularly dangerous because the hematoma may expand rapidly and compromise the airway.
How do you treat a hematoma?
Treatment of a hematoma depends on its severity. Small hematomas may resorb after a few days. More severe hematomas that continue to enlarge may require surgery to drain the accumulated blood and/or control any bleeding vessels and reclose the surgical site. A common complication of all hematomas is the risk of infection. Since there is no blood supply to a hematoma (it is a collection of old blood), there is a risk of bacteria colonizing the site. Surgical incision separation and delayed healing may also occur if the hematoma is large enough to compress tissues and prevent oxygen from reaching the surrounding tissue.
What is a seroma?
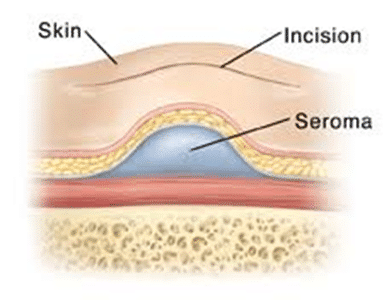 A seroma is a sterile collection of fluid under the skin, usually at the site of a surgical incision. Fluid builds up under the skin where tissue was removed. The formation of seromas is the body’s response to dead space within tissue that was attached to something before surgery. It may form soon after your surgery or up to 1 to 2 weeks after your procedure. It may appear as a swollen lump and feel tender or sore.
A seroma is a sterile collection of fluid under the skin, usually at the site of a surgical incision. Fluid builds up under the skin where tissue was removed. The formation of seromas is the body’s response to dead space within tissue that was attached to something before surgery. It may form soon after your surgery or up to 1 to 2 weeks after your procedure. It may appear as a swollen lump and feel tender or sore.
What are common treatments for a seroma?
A small seroma is not dangerous. Depending on its size and your symptoms, it may not need to be treated. The seroma may go away on its own within a few weeks or months. Your body slowly absorbs the fluid. No medicine will make it go away faster. But if you have a large seroma or if it’s causing pain, your healthcare provider may drain it. This is done with a syringe and needle. Or the provider may put in a drain. Seromas can return and may need to be drained multiple times. In some cases, it can become infected or turn into an abscess. Rarely, you may need a minor procedure to remove the seroma. Long-term problems from a seroma are rare.
What are some complications that can arise from a post-surgical hematoma or seroma?
Hematomas and seromas may increase the length of hospitalization and cause delayed healing, surgical site infection, and abnormalities in scarring. Therefore, following your healthcare provider’s instructions is very important.
To learn more about Sanara MedTech products, please visit. https://sanaramedtech.com/surgical/




