Preventing a Diabetic Foot Ulcer: What Are Simple Steps Every Patient Can Take?
The concern of a diabetic foot infection is something that is foremost in the minds of many diabetic patients. Educating diabetic patients about this potential problem Is imperative as a component of prevention or to at least detect complications in a wound before it becomes serious.
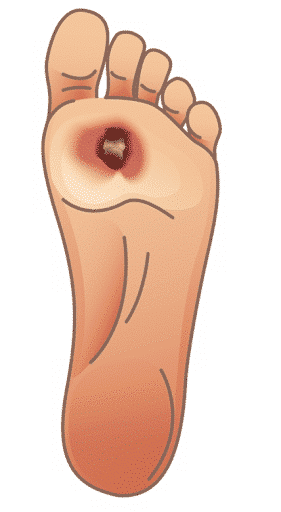
Diabetic patients are at high risk for infection for many reasons. The immune system of the diabetic patient may not function as well as the non-diabetic patient, especially if they have an elevated blood glucose or HgbA1C level. Impaired circulation (often associated in patients with diabetes) also impairs the fight against infection. In fact, infection in the presence of poor circulation greatly increases the chances of gangrene. Infection and gangrene in the diabetic patient may result in amputation. Regardless, at the root of the problem is a break in the skin. The skin is the body’s barrier against bacteria. Keeping the skin intact with routine foot care helps to avoid infectious complications. Tips for prevention include:
- Monitor your blood sugar control.
- Follow your healthcare provider’s foot care recommendations.
- Wear appropriate footwear and inspect feet daily. Avoid walking barefoot.
- Don’t use strong chemicals or cleansers. A gentle antimicrobial skin cleanser works well.
- Do not soak feet. Dry your feet, especially between the toes with regular bathing.
- Treat dry skin with recommended skin creams to prevent cracks.
- Follow instructions for care of insensate feet.
- Do not smoke.
- Exercise, following healthcare provider’s recommendations.
- Immediately report to the healthcare provider any breaks in the skin.
The greatest risk factor to diabetic foot injury and infection is the loss of protective sensation. Once sensation is lost, the skin can become injured without the patient feeling any pain. As already stated, a break in the skin is like opening Pandora’s Box. A diabetic patient who loses sensation is likely to be unaware of the skin break, prolonging the time period during which the area goes untreated. Once the infection develops, the patient still feels no pain and often continues to walk on the infected foot, delaying treatment even further. Walking on the infection compounds the problem by further compromising the surrounding tissues.
Patients need to be made aware that any breaks in the skin — whether from a wound, ingrown toenail, recent cut or scrape, callus, blister, heel crack or surgery — must be observed for signs of infection. To the general population, infections are generally painful. However, the diabetic patient may not feel pain, or the pain may not seem consistent with visual observations due to the sensation impairment associated with diabetic neuropathy.

- If the patient expresses feelings of lethargy, fever greater than 101, or general malaise, these may be indicative of infection.
- Blood sugars may become high and more difficult to control.
- The patient may notice redness, swelling or warmth surrounding the affected area.
- If the patient has a wound, an increase or change in drainage may be noted.
If an ulcer develops on the foot of a diabetic patient, the patient should see their healthcare provider immediately.
To learn more about products indicated for the treatment of diabetic foot ulcers, visit the Advanced Wound Care Products page on sanaramedtech.com.




