Pressure Ulcer/Injury Staging Classifications In Clinical Practice
What is a pressure injury?
The National Pressure Injury Advisory Panel (NPIAP) publishes evidence-based guidelines on the prevention and treatment of pressure injuries (formerly called pressure ulcers) as well as the International Pressure Injury Classification System. The definition of a pressure injury is localized damage to the skin or underlying soft tissue, usually over a bony prominence or related to a medical or other device. The injury may present as intact skin or an open ulcer and may be painful. It can result from intense and/or prolonged pressure that is significant enough to compromise tissue circulation. In addition to direct pressure, shear may also contribute to pressure injury development. Other factors that may impact the development of a pressure injury include changes in microclimate, nutrition, perfusion, co-morbid conditions and condition of the soft tissues.
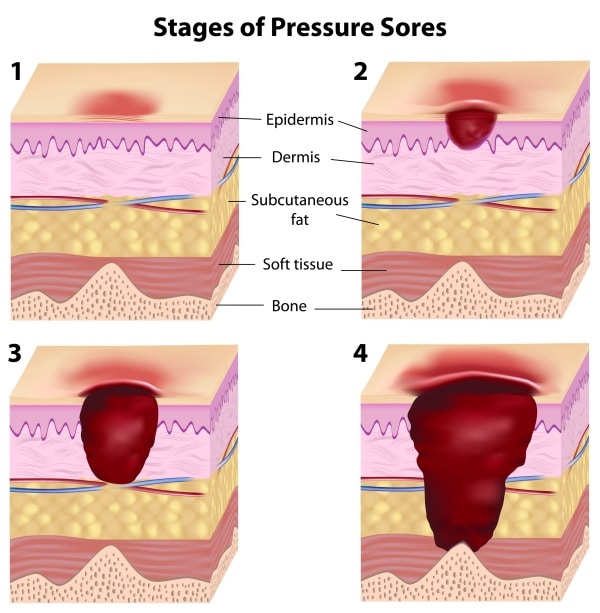
How are pressure injuries classified?
The International Classification System represents international consensus (NPIAP, the European Pressure Ulcer Advisory Panel, and the Pan Pacific Pressure Injury Alliance) on the classification of pressure injuries/ulcers. It describes and classifies localized injury to the skin and/or underlying tissue, as well as the categories of unstageable and suspected deep tissue injuries that describe pressure injuries for which the full extent of damage to the tissue and skin remains unknown. These stages include:
Stage 1

Intact skin with a localized area of non-blanchable erythema, which may appear differently in darkly pigmented skin. Presence of blanchable erythema or changes in sensation, temperature or firmness may precede visual cues. Color changes do not include purple or maroon discoloration which may be an indication of deep tissue injury.
Stage 2

Partial-thickness loss of skin with exposed dermis. The wound bed is viable, pink or red, moist and may also present as an intact or ruptured serum-filled blister. Fat (adipose) and deeper tissues are not visible. Granulation tissue, slough and eschar are not present.
Stage 3

Full-thickness loss of skin, in which fat may be visible in the injury and granulation tissue, and rolled wound edges (epibole) are often present. Slough and/or eschar may be visible. The depth of tissue damage varies by anatomical location. Those with a large body mass may exhibit deep wounds.
Stage 4

Full-thickness skin and tissue loss with exposed or directly palpable fascia, muscle, tendon, ligament, cartilage, or bone in the injury. Slough and/or eschar may be visible. Epibole, undermining and tunneling often occur. Depth varies by anatomical location.
Deep Tissue Injury

Intact or non-intact skin with localized area of persistent non-blanchable deep, red, maroon, purple discoloration or epidermal separation, revealing a dark wound bed or blood-filled blister. Pain and temperature change often precede skin color changes. Discoloration may appear differently in darkly pigmented skin. This injury results from intense and/or prolonged pressure and shear forces at the bone-muscle interface. The wound may evolve rapidly to reveal the actual extent of tissue injury or may resolve without tissue loss.

Unstageable
Full-thickness skin and tissue loss in which the extent of tissue damage within the injury cannot be confirmed because it is obscured by slough or eschar.
Medical Device Related Pressure Injury
Pressure injury that results from the use of devices designed and applied for diagnostic or therapeutic purposes. The resultant pressure injury generally conforms to the pattern or shape of the device. The injury should be staged using the staging system.
Mucosal Membrane Pressure Injury
A mucosal membrane pressure injury is found on mucous membranes with a history of a medical device in use at the location of the injury and due to the anatomy of the tissue, these injuries cannot be staged.
What if you don’t know the stage of an injury?
If you are unsure of the stage of an injury, don’t guess. Make sure you describe your assessment findings, including: injury/ulcer location, size (measured length, width and depth), tissue type(s), color, wound edges, any sinus tracts, undermining or tunneling, exudate (amount, type and odor) and periwound assessment of skin heat, tenderness, change in consistency or pain. Report this information to a wound specialist or provider to assist in the identification of the appropriate stage for the pressure injury.
How should you document a healing pressure ulcer?
Do not reverse stage when documenting a healing pressure injury/ulcer. The amount of tissue damaged remains the same, and granulation tissue is not the same as the original tissue. To document healing of a pressure injury, identify the highest level of staging and the status of that wound. For example, “healing stage 4 pressure injury with granulation tissue over x% of the wound bed,” or another example might be a “fully epithelialized (or closed) stage 3 pressure injury.”
How should the pressure injury staging classification be used?
It is important to use the pressure injury staging classification system as a component of the total patient and wound assessment in pressure injuries/ulcers and as a component in monitoring healing. The pressure injury/ulcer staging classification system is developed specifically to describe pressure impact on the skin and surrounding tissue, and cannot be used to categorize other wound etiologies.
For more information on products indicated for the treatment of pressure injuries, please visit https://sanaramedtech.com/wound-care/
References
NPIAP, 2016a. Accessed July 2021.




