Matrix-Derived Peptides Orchestrate a Wound Healing Symphony
What are the roles of matrix-derived peptides during surgical wound healing?

One might think of wound healing as a ballet of sorts, with extracellular matrix (ECM)-driven wound repair coordinated just as the conductor or ‘pitmaster’ controls the content and tempo of the score being played during a ballet or operatic performance. Along with the choreographers who set the movement of dancers on stage, and costume and set designers stage all the events from the opening act to the final curtain, timing and discipline dictate whether a fabulous or failing performance ensues. So, too, might be the case during the body’s responses to injury, where cellular signals and molecular cues control whether or to what extent repair and regeneration result in a well-healed surgical site.

A growing, compelling body of basic science and clinical evidence indicate that there exists a coordinated and well-controlled response to injury involving matrix-derived and wound healing peptides. Whether released naturally from the ECM through the action of endogenous metalloproteinases (MMPs) or delivered to the wound bed in the form of hydrolyzed collagen and collagen-derived peptides, these connective tissue or matrix-derived peptides act as molecular signaling entities or extrinsic matrix-derived components that orchestrate wound repair and tissue regeneration, representing key aspects of wound healing. Likely binding to specific receptors, either on the cell surface or within the cytoplasm, the peptide(s) activate or trigger signaling cascades that influence cell behaviors, including dermal and epidermal wound healing responses. Below are but a few key examples of matrix-derived peptide coordination of wound repair and healing.
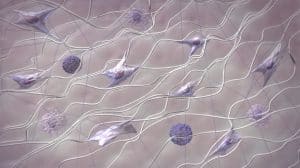
Promoting Cell Migration and Proliferation: Paving the Way for Tissue Reconstruction
Matrix-derived peptides play a crucial role in promoting cell migration and proliferation, two fundamental responses essential for tissue reconstruction. Peptides such as collagen fragments and fibronectin peptides stimulate the movement of fibroblasts, keratinocytes, and endothelial cells within the wound site.
Modulating Inflammation: Maintaining a Balanced Healing Environment
Inflammation is an integral part of wound healing, facilitating the clearance of debris and pathogens. However, excessive inflammation can hinder tissue repair. Matrix-derived peptides modulate host immunity and inflammation by influencing the recruitment and activation of inflammatory cells modifying healing. Peptides derived from ECM-derived macromolecules like decorin, a collagen-associated extracellular matrix proteoglycan and laminin, major constituent of the epidermal and microvascular basement membranes foster the recruitment of macrophages, while others, such as hyaluronan fragments suppress the activation of inflammatory cells.
Regulating Angiogenesis: Restoring Blood Supply for Tissue Rejuvenation
Angiogenesis, the formation of new blood vessels, is essential for providing oxygen and nutrients to the healing wound. Matrix-derived peptides, such as those collagen-derived and collagen-associated peptide discovered by our team stimulate the proliferation and migration of dermal microvascular endothelial cells, which promote the formation of new blood vessels, enhance the exchange of nutrients for metabolites while promoting dermal and epidermal remodeling and wound repair.
Enhancing ECM Remodeling: Recreating Tissue Architecture
The dynamic process of ECM synthesis and degradation is crucial for restoring tissue architecture and function. Matrix-derived peptides are not only produced through the concerted action and activity of matrix metalloproteinases (MMPs), enzymes responsible for ECM breakdown and matrix-derived peptide production; but, similarly, peptides such as tissue inhibitors of metalloproteinases (TIMPs), e.g., TIMP-1 and TIMP-2 inhibit MMP activity. This delicate balance of ECM synthesis and degradation ensures the formation of a well-organized and functional ECM, dermal compartment, and overlying epidermis through their concerted action on the remodeling basement membrane that controls microvascular and epithelial repair and regeneration.
Peptide-Based Scaffolds: Providing a Structural Framework for Tissue Regeneration
Peptide-based scaffolds, composed of naturally occurring and/or combinations of synthetic matrix-derived peptides, provide a structural framework for tissue regeneration. These scaffolds can be engineered to mimic the ECM architecture and while incorporating key molecular signaling entities, e.g. bioactive peptides that promote cell adhesion, migration, and proliferation.
Peptide-Based Therapeutics: Delivering Signaling Cues for Enhanced Wound Healing
Peptide-based therapeutics administered topically can deliver key signals or molecular cues that enhance wound healing. These peptides can modulate inflammation, promote angiogenesis, or regulate ECM remodeling, therein fostering or promoting tissue repair and regeneration.
Matrix-Derived Peptides Orchestrate a Symphony of Wound Healing
Matrix-derived peptides, whether endogenously created in situ through the action of MMPs or added exogenously as hydrolyzed collagen and collagen-derived peptides, act as signaling molecules, playing pivotal roles in orchestrating wound repair and regeneration. These peptides modulate a multitude of cell behaviors, temporally and spatially, regulating inflammation, angiogenesis, and ECM remodeling. All these peptide-driven molecular and cellular events contribute to the repair and restoration of tissue structure and function. Without question, the advancement of peptide-based scaffolds and therapeutics hold immense promise for accelerating wound healing while significantly improving clinical outcomes.
To learn more about surgical and wound care products that contain hydrolyzed collagen, visit: CellerateRX® Surgical Hydrolyzed collagen | Sanara MedTech Inc.
References
Matrix-derived Peptides Promote Wound Repair and Tissue Regeneration.
- Demidova-Rice TN, Durham JT, Herman IM. 2012. Wound Healing Angiogenesis: Innovations and Challenges in Acute and Chronic Wound Healing. Adv Wound Care (New Rochelle). Feb;1(1):17-22. doi: 10.1089/wound.2011.0308. PMID: 24527273 Free PMC article. Review.
- Sharma S, Rai VK, Narang RK, Markandeywar TS. 2022. Collagen-based formulations for wound healing: A literature review. Life Sci. Feb 1;290:120096. doi: 10.1016/j.lfs.2021.120096. Epub 2021 Oct 26. Erratum in: Life Sci. 2022 May 15;297:120436. PMID: 34715138.
- Dulmovits BM, Herman IM. 2012. Microvascular remodeling and wound healing: a role for pericytes. Int J Biochem Cell Biol. Nov;44(11):1800-12. doi: 10.1016/j.biocel.2012.06.031. Epub 2012 Jun 28. PMID: 22750474 Free PMC article. Review.
- Weigelt MA, Lev-Tov HA, Tomic-Canic M, Lee WD, Williams R, Strasfeld D, Kirsner RS, Herman IM. 2021. Advanced Wound Diagnostics: Toward Transforming Wound Care into Precision Medicine. Adv Wound Care (New Rochelle). 2022 Jun;11(6):330-359. doi: 10.1089/wound.2020.1319. Epub 2021 Jul 21. PMID: 34128387 Free PMC article. Review.
- Demidova-Rice TN, Hamblin MR, Herman IM. 2012. Acute and impaired wound healing: pathophysiology and current methods for drug delivery, part 2: role of growth factors in normal and pathological wound healing: therapeutic potential and methods of delivery. Adv Skin Wound Care. Aug;25(8):349-70. doi: 10.1097/01.ASW.0000418541.31366.a3. PMID: 22820962 Free PMC article. Review.
- Demidova-Rice TN, Hamblin MR, Herman IM. 2012. Acute and impaired wound healing: pathophysiology and current methods for drug delivery, part 1: normal and chronic wounds: biology, causes, and approaches to care. Adv Skin Wound Care. 2012 Jul;25(7):304-14. doi: 10.1097/01.ASW.0000416006.55218.d0. PMID: 22713781 Free PMC article.
- Borenstein, Jeffrey T., Katie Megley, Kimberly Wall, Eleanor M. Pritchard, David Truong, David L. Kaplan, Sarah L. Tao, and Ira M. Herman. 2010. “Tissue Equivalents Based on Cell-Seeded Biodegradable Microfluidic Constructs” Materials 3, no. 3: 1833-1844. https://doi.org/10.3390/ma3031833
- Schultz GS, Davidson JM, Kirsner RS, Bornstein P, Herman IM. 2011. Dynamic reciprocity in the wound microenvironment. Wound Repair Regen. 2011 Mar-Apr;19(2):134-48. doi: 10.1111/j.1524-475X.2011.00673.x. PMID: 21362080 Free PMC article. Review.
- Sheets AR, Demidova-Rice TN, Shi L, Ronfard V, Grover KV, Herman IM. 2016. Identification and Characterization of Novel Matrix-Derived Bioactive Peptides: A Role for Collagenase from Santyl® Ointment in Post-Debridement Wound Healing? PLoS One. 2016 Jul 26;11(7):e0159598. doi: 10.1371/journal.pone.0159598. eCollection 2016. PMID: 27459729 Free PMC article.
- Herman IM, Leung A. 2009. Creation of human skin equivalents for the in vitro study of angiogenesis in wound healing. Methods Mol Biol. 2009;467:241-8. doi: 10.1007/978-1-59745-241-0_14. PMID: 19301675.
- Riley KN, Herman IM. 2005. Collagenase promotes the cellular responses to injury and wound healing in vivo. J Burns Wounds. 2005 May 17;4:e8. PMID: 16921413 Free PMC article.
- Demidova-Rice TN, Geevarghese A, Herman IM. 2011. Bioactive peptides derived from vascular endothelial cell extracellular matrices promote microvascular morphogenesis and wound healing. Wound Repair Regen. 2011 Jan-Feb;19(1):59-70. doi: 10.1111/j.1524-475X.2010.00642.x. Epub 2010 Dec 6. PMID: 21134032 Free PMC article.
- Herman IM. 1993. Molecular mechanisms regulating the vascular endothelial cell motile response to injury. J Cardiovasc Pharmacol. 1993;22 Suppl 4:S25-36. doi: 10.1097/00005344-199322004-00005.PMID: 7523770
The Science of Collagen-Hydrolyzed Collagen
- Arely León-López , Alejandro Morales-Peñaloza , Víctor Manuel Martínez-Juárez , Apolonio Vargas-Torres , Dimitrios I. Zeugolisand Gabriel Aguirre-Álvarez. 2019. Hydrolyzed Collagen—Sources and Applications. Molecules 2019, 24, 4031.https://doi.org/10.3390/molecules24224031
- Mian M et al. 1992. Collagen as a pharmacological approach in wound healing. Int J Tissue React. 114 Suppl:1-9https://pubmed.ncbi.nlm.nih.gov/1639580/’
- Chung L, Dinakarpandian D, Yoshida, N, Fields JLL, Fields GB, Visse R, and Nagases H. 2004. Collagenase unwinds triple helical collagen prior to peptide bond hydrolysis. The European Molecular Biology Organizational Journal. Vol23, pp3020https://www.ncbi.nlm.nih.gov/pmc/articles/PMC514933/pdf/7600318a.pdfHydrolyzed Collagen for Wound Application in Peer Reviewed Journals(CellerateRX specific)
- Hochstein, A and Savage, A. 2013. Examining the Effectiveness of Type 1 Activated Hydrolyzed Collagen in Wound Care. Today’s Wound Clinic. 2013:7(7). (CellerateRX Surgical) https://www.hmpgloballearningnetwork.com/site/twc/articles/examining-effectiveness-type-1-activated-hydrolyzed-collagen-wound-care
- Newman, M, Bratta L , Swartz K. 2008. Activated, Type I Collagen (CellerateRx) and Its Effectiveness in Healing Recalcitrant Diabetic Wounds: A Case Presentation. Adv in Skin and Wound Care. 21(8)370-374.https://pubmed.ncbi.nlm.nih.gov/18679085/Moore J. Examining the Potential of Collagen Powders in the Diabetic Foot. Podiatry Today May 2015:28(5); 18-22.https://www.hmpgloballearningnetwork.com/site/podiatry/examining-potential-collagen-powders-diabetic-foot
- Evans DC and Evans BG. 2018. The Effects of Platelet Rich Plasma and Activated Collagen on Wound Healing in Primary Total Joint Arthroplasty. Orthopedics. 2018; 41(2):e262-e267.(CellerateRX Surgical Powder)https://pubmed.ncbi.nlm.nih.gov/29451945/
- Dickerman R, Ashley SRNP, Winters K. 2017. Operative Closure Technique Utilizing Bovine Collagen Fragments in a Prospective Analysis of 102 Consecutive Neurosurgery Patients. JSM Neurosurg Spine :5(2): 1088.(CellerateRX Surgical Powder) https://www.jscimedcentral.com/Neurosurgery/neurosurgery-5-1088.pdf
- Hotchkiss WR. 2021. Retrospective Study to Evaluate the Use of Type 1 Bovine Hydrolyzed Collagen to Support Surgical Wound Healing After Spinal Surgery. JSM Neurosurg Spine (1):1103.https://www.jscimedcentral.com/Neurosurgery/neurosurgery-8-1103.pdf
- Gitelman A (2022) The Use of Sterile Bovine Type 1 Hydrolyzed Collagen to Support Surgical Wound Management: A Case Series. JSM Neurosurg Spine 9(1): 1108.
- Kumar M, Banerjee P, Das A, Singh K, Guith T, Kacar S, Gourishetti K, Sen CK, Roy Khanna S. 2023. Hydrolyzed Collagen Powder Dressing Improves Wound Inflammation, Perfusion, and Breaking Strength of Repaired Tissue. Adv Wound Care (New Rochelle). Sep 13. (e pub Aug 2023) doi: 10.1089/wound.2023.0065




