How Do Wounds Heal? A Guide to the Phases of Wound Healing for Clinicians and Patients
What are the phases of wound healing?
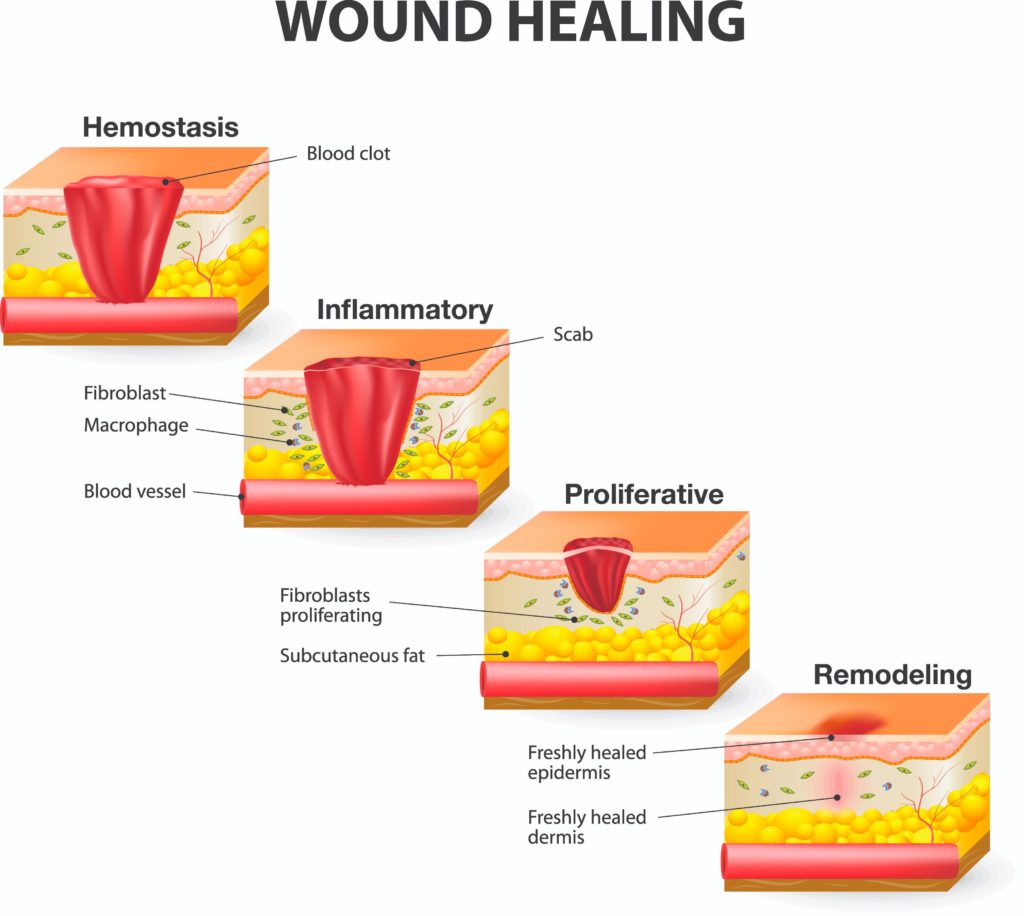
The body goes through a series of overlapping phases to achieve wound healing after a full thickness skin injury. These phases include Hemostasis, Inflammation, Proliferation and Maturation. During each phase there is a complex interaction between numerous cell types and cell mediators. Most wounds proceed uneventfully through these phases toward healing, but wounds that become chronic are those that are typically arrested in one of these phases. Addressing the factors that cause the wound to be stagnant in a particular phase is key to resuming the healing process.
What is the first phase of wound healing?
The first phase of wound healing is Hemostasis. This initial phase is one of vasoconstriction of blood vessels, collagen activation of coagulation factors, and platelet aggregation that stops bleeding. This is the formation of a fibrin clot which provides the initial wound healing process and prevents excessive loss of blood and body fluids.
What is the inflammatory phase of wound healing?
This is followed by the next phase which is referred to as the Inflammatory phase due to the influx of inflammatory cells that work to remove cellular debris and bacteria, promote collagen degradation, and stimulate surrounding vessels to dilate and become more permeable. The dilation of the surrounding vessels increases the serous fluid in the wound bed, and causes the wounded area to appear reddened, slightly swollen and warm to the touch with varying amounts of drainage. The cellular, protease and other key elements of this phase are necessary for normal wound healing. However, if this phase is prolonged, incomplete, or results in an uncoordinated physiologic response, it often results in pathologic inflammation and can delay the healing process.
What is the proliferation phase of wound healing?
The next phase, Proliferation, is tightly connected with the inflammatory response, and also plays an important role in resolving inflammation. During the Proliferative phase, the wound deficit is filled with new granulation tissue, capillary networks and covered with epithelium. New granulation tissue occurs concurrently with collagen synthesis.
What is the maturation phase of wound healing?
The last phase is Maturation. This phase is identified by a closed wound that continues to strengthen through connective tissue collagen synthesis. Collagen matures over time and provides tensile strength to the healing wound. After healing, scar tissue tensile strength is approximately 80% of the non-wounded tissue. The Maturation phase continues for up to a year or longer after injury.
What factors impact the phases of wound healing?
Many factors may impact the phases of wound healing. Primary factors that impair the healing process include poor perfusion, high bioburden or biofilm, uncontrolled co-morbid disease, malnutrition, or smoking. Local factors that can impair the healing process include pressure, excessive swelling, maceration and dehydration. Effective wound management includes addressing any underlying disease or factors that can impair healing, defending the intact skin and wounded area from bioburden and infection, removing any devitalized tissue from the wound bed, and providing a wound environment with adequate moisture and support.
To learn more about products indicated for the management of acute and chronic wounds, please visit: https://sanaramedtech.com/wound-care/





