Assessment and Management of Wound Drainage (Exudate)
What is wound exudate?

The body produces fluid to an injured site for appropriate and timely healing as a normal response to tissue damage. The fluid that exudes out of a tissue or its capillaries because of injury or inflammation is known as exudate. This is different from fluid that occurs as a result of disturbances of hydrostatic or colloid osmotic pressure (not inflammation) which is known as transudate. Transudate may accumulate in tissues and cause edema. It typically has a lower protein content, lower specific gravity, and fewer cell counts than exudate. It is also relatively clearer than exudate in appearance.
What are the benefits of wound exudate?
Exudate fluid provides a variety of growth factors, proteins, enzymes and a cellular-rich source to prevent tissues from drying out, provide immune dense functions, stimulate cellular growth and regulation and support tissue remodeling. Excessive or insufficient exudate or changes in the biochemical composition of the fluid may result in delayed healing and chronic wounds.
How should you assess and document wound exudate?
When assessing exudate, the fluid consistency — such as watery or viscous — should be documented. Any odor, such as sweet, fruity, fishy, ammonia-like, and foul, should also be described.

Exudate should also be documented by common terminology that includes:
- Serous – Clear, watery drainage
- Sanguineous (or bloody) – Red, bloody-looking watery drainage
- Serosanguinous – Pink/reddish, watery drainage
- Purulent (or pus) – Yellow, green, tan, creamy or other drainage that is also cloudy; may be watery or viscous
The amount of drainage should also be noted. While there is no standard amount of exudate production or method for measuring the rate of production, monitoring the exudate amount is important to support wound healing assessment and to support dressing selection and reimbursement requirements.
What are some common terms used for documenting wound exudate?
Common terms to document the amount of exudate include:
- None– Wound tissue appears dry
- Scant– Wound tissue is moist, but no measurable exudate
- Small– Wound tissues are wet and moisture is evenly distributed in the wound (typically drainage involves ≤25% of the dressing)
- Moderate -Wound tissues saturated; drainage may or may not be evenly distributed in the wound; drainage involves >25% to ≤75% of the dressing
- Large – Wound tissues bathed in fluid; drainage freely expressed; may or may not be evenly distributed in the wound; drainage involves >75% of the dressing
- Copious – Wound tissues bathed in fluid and freely draining with >75% saturated superabsorbent dressings
What is the relationship between the amount of wound exudate and healing?
Maintaining an environment for wound healing involves a moist environment. It is important for clinicians to be able to assess whether the amount of exudate being produced by a wound is normal, too low or too high, and, importantly, whether it has changed since the previous assessment. The amount and characteristics of wound exudate should be documented with each wound assessment and/or dressing change in the medical record. The exudate amount typically diminishes as healing progresses.
Addressing the underlying cause and comorbid conditions that are impacting wound healing and exudate production needs to be a priority. Systemic conditions such as malnutrition, dehydration, congestive heart failure, vascular compromise, renal disease or diabetes may impact the exudate fluid composition or amount. Local conditions such as biofilm infection or excess matrix metalloproteinases may also be a factor.
What are some treatment approaches for exudating wounds?
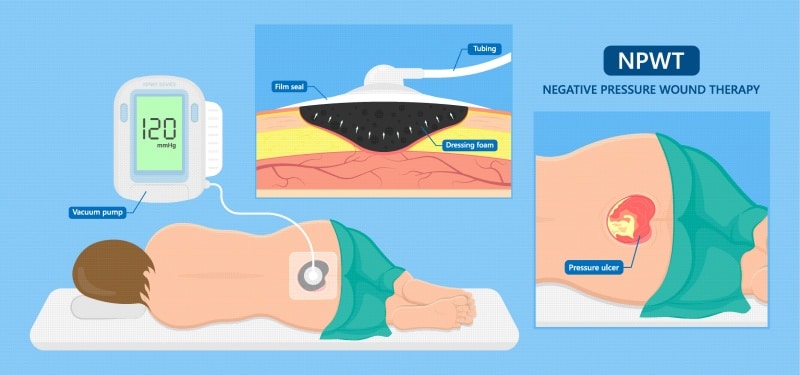
Advanced wound dressings, pouches and therapies (e.g. NPWT) assist in the management of exudate amounts. These items function to either absorb/remove excessive moisture, add moisture to prevent desiccation, or maintain the existing moisture balance. Adequate management of wound exudate is critical to managing an increased bioburden in the wound. Selection of dressings and exudate management devices should match the characteristics of the wound, such as amount of exudate, location and composition. The periwound tissue should also be protected when considering the impact of exudate management. Wound healing and the resulting exudate are dynamic in that they change over time, which means dressings from multiple functional categories may be appropriate for a single wound during its overall course of treatment.
Exudate also impacts an individual’s quality of life. Ineffective exudate management can lead to odor, maceration, increased frequency of dressing changes and thereby impact physical, social and lifestyle needs. Quality of life should be considered when addressing approaches in exudate management.
In summary, the goal of exudate assessment and management is to optimize the wound environment, protect healing tissue and surrounding skin, and implement a plan that supports or improves the patient’s quality of life. On-going assessment and documentation of exudate characteristics and treatment plans should be communicated in the medical record. Treatment plans and product selection for wound exudate management should include not only appropriate and effective therapies based on the individual wound, but take into consideration cost-effectiveness and overall patient impact.
To learn more about products indicated for the management of acute and chronic wounds as well as varying levels of wound exudate, please visit https://sanaramedtech.com/wound-care/
References:
Lampe KE. Assessing the Patient – The General Evaluation in MuCulloch JM and Kloth LC Wound Healing Evidence-Based Management. 4th Edition. 2010; 80-81.
World Union of Wound Healing Societies (WUWHS) Consensus Document. Wound exudate: effective assessment and management Wounds International, 2019.




