A Silent Architect of Post-Surgical Healing: The Extracellular Matrix
In surgical tissue recovery, focus is on controlling infection, managing inflammation, and ensuring wound closure. Beneath the surface—anatomically and biologically— the extracellular matrix (ECM) is undergoing remodeling ensure long-term tissue integrity. The ECM is a dynamic, biologically active network that orchestrates the entire process of tissue repair, remodeling, and regeneration after surgery. The ECM’s role in healing is the bidirectional, continuous interaction between cells and their surrounding matrix, known as dynamic reciprocity. This process defines how cells respond to ECM cues while simultaneously modifying the ECM through the secretion of enzymes, growth factors, and structural proteins. These dynamic interactions help regulate cellular behaviors such as migration, proliferation, and differentiation throughout wound healing. The interplay between the cells and ECM define the quality, integrity, and restoration of the tissue, directly influencing whether healing is functional and regenerative or leads to fibrosis, adhesions, or chronic complications.
What is the Extracellular Matrix?
The ECM is a complex network of structural proteins, glycoproteins, and proteoglycans, collectively providing mechanical strength, tissue integrity, biochemical signaling to resident and infiltrating cells, structural guidance for cell migration and organization, and reservoirs for growth factors and cytokines, known as matrikines.
Each tissue type has its own unique ECM composition tailored to its mechanical and functional needs, whether in skin, bone, or organs.
The ECM’s Role in Healing: A Stepwise Orchestration
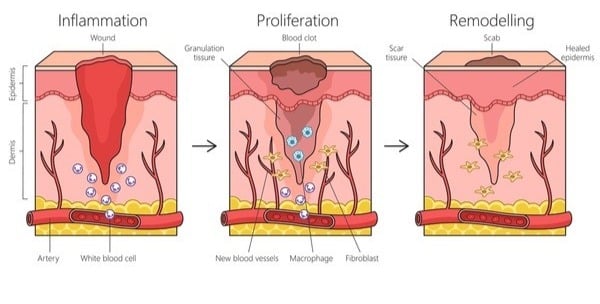
After surgery, the body enters a highly regulated, overlapping sequence of events involving hemostasis, inflammation, proliferation, and remodeling. The ECM is an integral function, actively participating in each phase:
- Hemostasis & Early Inflammation: fibrinogen activation, platelet aggregation, and histamine release acts to mobilize immune cells and recruit inflammatory mediators.
- Cell Migration & Proliferation: Provisional matrix proteins and cytokine secretion guide fibroblasts and endothelial cells to the wound site, promoting angiogenesis and granulation tissue.
- Remodeling: Fibroblasts lay down new collagen, while matrix metalloproteinases (MMPs) carefully balance remodeling of ECM components to restore structure.
The quality of ECM remodeling determines whether a tissue returns to semblance of its original architecture—or develops disorganized, fibrotic scar tissue.
When ECM Healing Goes Wrong
Surgical complications often trace back to disrupted ECM dynamics, thus the quality of tissue healing is crucial to the success of the procedure, the life of the repair, and outcomes for the patient. The impact of a poorly functioning ECM can lead to loss of mechanical strength, dehiscence, and, ultimately, development of chronic wounds. Poor cellular and extracellular management can be attributed to several factors, including, excessive ECM degradation by presence of overactive matrix metalloproteinases (MMPs), inadequate collagen cross-linking that results in mechanically weak scar tissue, and overproduction of fibrotic ECM, which can lead to hypertrophic scars, keloids, adhesions, or contractures. Additionally, an altered or dysfunctional ECM environment impairs angiogenesis and delays epithelialization, further hindering proper healing. In surgical cases in which implants are utilized, poor ECM regeneration can compromise bony integration, graft success, or tissue functionality.
Therapeutic Strategies to Support ECM Integrity
Modern approaches to surgical recovery are increasingly ECM-centric, as researchers are increasingly aware of the central role in surgical recovery. Scaffolds, such as decellularized ECM, and engineered biomaterials are designed to provide a provisional structure that mimics native tissue architecture, supporting cellular infiltration and accelerating matrix remodeling. Adjunctive therapies, like negative pressure wound therapy (NPWT), contribute by mechanically modulating the wound microenvironment, promoting perfusion, removing contaminants, and managing wound exudate to create optimal healing conditions. Additionally, topical agents are being developed and utilized to directly influence ECM-related processes, including the regulation of MMP activity, stimulation of collagen synthesis, and modulation of fibroblast gene regulation, all of which are critical for balanced and functional tissue repair.
Measuring Success: It’s About More Than Closure
Traditionally, surgical healing is judged by wound closure, but the quality of the ECM repair success lies in functional tissue restoration:
- Is mechanical strength restored?
- Has native architecture been restored?
- Is the scar biology restored?
- Are cells receiving the right signals for long-term homeostasis?
Conclusion: Healing Beyond the Surface
The extracellular matrix is more than structure—it’s strategy. It facilitates an appropriate immune response, guides cellular players, and ultimately defines the quality of tissue healing. Understanding and supporting ECM restoration in surgical patients is the key to moving from just closing wounds to regenerating functional tissue. To learn more about an extracellular matrix product, please visit FORTIFY TRG Tissue Repair Graft® | Sanara MedTech Inc..
References:
- Diller RB, Tabor AJ. The Role of the Extracellular Matrix (ECM) in Wound Healing: A Review. Biomimetics (Basel). 2022;7(3):87. Published 2022 Jul 1. doi:10.3390/biomimetics7030087
- Alfonso et al. Decellularized Tissues for Wound Healing: Towards Closing the Gap Between Scaffold Design and Effective Extracellular Matrix Remodeling. Frontiers in Bioengineering and Biotechnology. 2022;(10). Published 2022 Feb 15. doi:10.3389/fbioe.2022.821852
- Xue M, Jackson CJ. Extracellular Matrix Reorganization During Wound Healing and Its Impact on Abnormal Scarring. Adv Wound Care. 2015;4(3):119-136. doi:10.1089/wound.2013.0485
- Quondamatteo et al. Extracellular matrix-inspired biomaterials for wound healing. Mol Biol Rep. 2024; 51: 830. doi: 10.1007/s11033-024-09750-9
- Rousselle et al. Extracellular matrix contribution to skin wounds re-epithelialization, Matrix Biol. 2019; 75-76: 12-26. doi: 10.1016/j.matbio.2018.01.002
- Schultz et al. Dynamic reciprocity in the wound microenvironment. Wound Repair Regen. 2011;19(2):134-148. doi:10.1111/j.1524-475X.2011.00673.x




